Understanding Utrogestan
Utrogestan is a medication that contains micronised progesterone derived from plants. It’s biochemical structure is identical to the progesterone produced in a woman’s ovaries. Hence it’s often described as body-identical.
Progesterone is a type of progestogen hormone, and an important element of Hormone Replacement Therapy (HRT) for women who haven’t had a hysterectomy.
Why is progesterone important?
Progesterone is produced by the corpus luteum during the second (luteal) part of the menstrual cycle. It plays an important role in maintaining the lining of the womb in preparation for implantation of a fertilised egg. However, if implantation doesn’t occur, when progesterone levels drop at the end of the luteal phase the womb lining sheds and this is what we see as a period.
Most perimenopause and menopause symptoms are due to insufficient circulating levels of oestradiol, the predominant ovarian oestrogen. As such, it’s oestradiol that is most helpful in managing the difficult symptoms women can experience at these times.
However, oestradiol is also what causes womb lining to thicken (ready for implantation). Without additional progesterone womb lining may thicken too much and lead to abnormal bleeding or even womb cancer. Therefore, if a woman has her womb and requires HRT, a progestogen is a critical element to protect the womb lining (endometrium) and reduce cancer risk. This is often called endometrial protection.
How should Utrogestan be taken?
The form of Utrogestan licensed for HRT is Utrogestan 100mg oral capsules. There is a vaginal form that is a different strength and licensed for use in fertility and pregnancy.
It should be taken on an empty stomach, ideally 2 hours after food, last thing before sleep. This is because many women find the capsules provide a mild sedation. This can be helpful in those who struggle with sleep.
If it’s been more than 12 months since your last period, a woman should use continuous combined HRT, using their choice of oestradiol alongside 1 x 100mg capsule of Utrogestan continuously so as not to trigger any bleeding. The licence for the medication is to take it for 25 out of 28 days but there should be no harm in taking it every night.
If it’s been less than 12 months since your last period, or you’re still having regular or irregular periods in perimenopause, the recommendation is to use a sequential combined regime to trigger a regular “shedding” of the womb-lining as a monthly withdrawal bleed. Alongside daily/continuous oestradiol, 2x100mg capsules of Utrogestan are taken for 12-14 nights of each 28 day cycle. The licence states they should be taken from day 15 to day 26 (inclusive). If this is difficult to remember you may find it easier to start on the first of each month and take 2x100mg every night for 14 nights.
As the action of Utrogestan is to control the womb lining, when the capsules are stopped each month a withdrawal bleed should occur.
In women on doses of oestrogen higher than 2 pumps of Oestrogel (or equivalent) the dose of Utrogestan may need to be increased to 200mg continuously or 300mg sequentially.
What side effects can I expect with Utrogestan?
It’s common to experience irregular bleeding or a change to monthly bleeding pattern initially with Utrogestan. This normally settles within the first 3-6 months. Some women find that Utrogestan is simply not effective enough to control bleeding symptoms and this is a common reason for switching to an alternative.
If you’re using Utrogestan continuously and you have ongoing unscheduled bleeding after 6 months, you must speak to your doctor. If using it sequentially and bleeding more than monthly, or if bleeds are heavy again, please consult your doctor.
Other common side effects include headaches, bloating and lower abdominal discomfort. Some women also find it impacts mood and emotional wellbeing. This is a common side effect of all progestogens and generally Utrogestan is better tolerated in this regard compared to older synthetic progestogens such as norethisterone, levonorgestrel or medroxyprogesterone acetate.

If any side effects do not settle, then you should consult your doctor as Utrogestan can be used in an alternative way, albeit off-licence. Sometimes switching to a synthetic progestogen that is delivered via the skin in combined patches or directly into the womb (Mirena-IUS) can minimise systemic side effects from oral use.
Why should I stick with Utrogestan?
There’s a correlation between the use of combined HRT (oestrogen + progestogen) and breast cancer and this relationship is the subject of much research. Recent studies indicate that using Utrogestan is associated with a lower risk of breast cancer than synthetic progestogens such as those mentioned above.
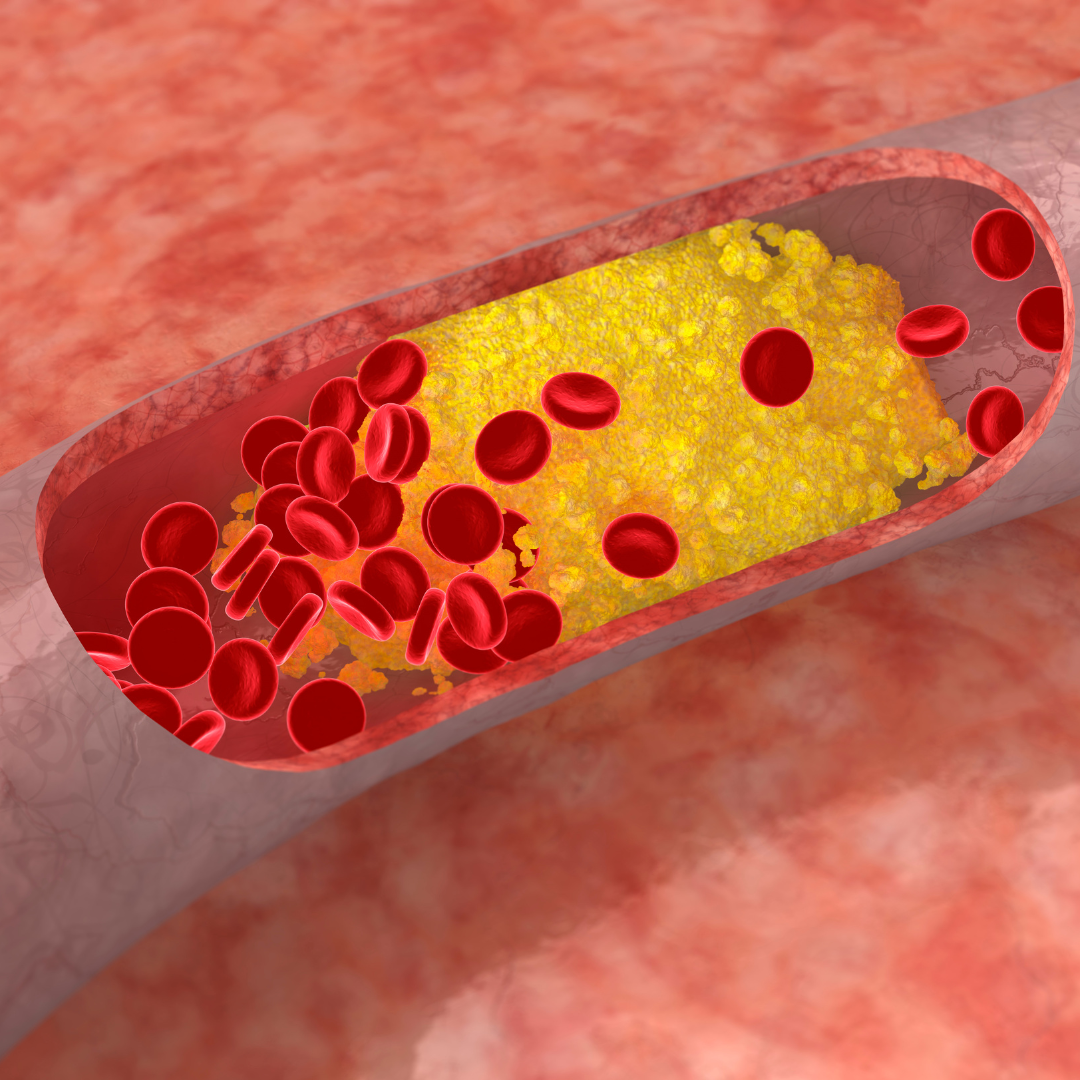
Some older progestogens are also associated with an increased risk of blood clots, but recent research indicates there is no increased risk of blood clots with use of Utrogestan. There is also no increase in the risk of blood clots when Oestradiol is delivered via the skin (transdermal) in spray, gel or patch form.
Consequently, current guidelines support the use of transdermal Oestradiol with oral Utrogestan as a useful starting point for women who require HRT and haven’t had a hysterectomy. However, there is no one size fits all in good menopause care, so although recommended as the safest combination it may not be the most appropriate combination for all women.
Useful Links
Besins Healthcare | Utrogestan website www.utrogestan.co.uk
Patient Information Leaflet | Utrogestan 100mg capsules www.medicines.org.uk
About Dr Fionnuala Barton
Dr Fionnuala Barton is a GP, Women's Health Doctor and registered member of the British Menopause Society.
She is passionate about optimising physical and emotional wellness for women at all stages of life and has particular interest in early recognition and management of perimenopausal and menopausal symptoms, POI, PMS and PMDD.
She draws on a wealth of clinical and personal experience to provide an empathetic, holistic, personalised and proactive, evidence-based hormone therapy approach. Appointments can be be booked directly with her at www.themenopausemedic.com.
www.harleystathome.com | Instagram @harleystreetathomemenopause
Facebook: Search Harley Street at Home: Diagnosis, Symptoms & Treatments or Harley St at Home: Lifestyle, Self-Care and Lifestyle to join our private community