Metabolic Syndrome in Menopause
Many of us are aware of lifestyle medical conditions such as type 2 diabetes and cardiovascular disease. However, more often than not, metabolic syndrome isn’t mentioned. This is despite one in three adults aged over 50 in the UK being impacted (1). By definition, metabolic syndrome is a collection of risk factors, including insulin resistance, high blood pressure, being overweight and unfavourable blood lipid levels, which increase your risk of developing type 2 diabetes or cardiovascular disease (1,2).
What is insulin resistance?
Insulin is a hormone produced in the pancreas. This hormone helps remove sugar from blood, into cells, where it can be used for energy (3).
Unfortunately, there can be scenarios where someone’s body doesn’t respond effectively to insulin. This means that sugar isn’t removed from blood, resulting in high blood sugar levels. As a result, the pancreas tries to compensate by producing more and more insulin. While this might sound useful, remember that the body isn’t responding very well to this insulin. This puts the pancreas under immense pressure and can consequently damage the pancreas, including the potential for it to stop producing insulin altogether (2).
High blood sugar levels, also known as hyperglycaemia, can have adverse consequences. This includes damage to blood vessels, which can lead to issues with eyes, nerves and kidneys. Type 2 diabetes may also occur when blood sugar levels reach high enough levels (4). Furthermore, type 2 diabetes is a risk factor for cardiovascular disease.

Why do blood lipid levels matter?
Our blood contains different types of lipids - tiny molecules that play a big role in many functions of our body. But that doesn’t mean the more the merrier.
Triglycerides are a type of blood lipid which provide energy. However, in excess, triglycerides can promote cardiovascular disease. Risk factors for high triglyceride levels include genetics, but also a high saturated fat intake, alcohol and a sedentary lifestyle (5).
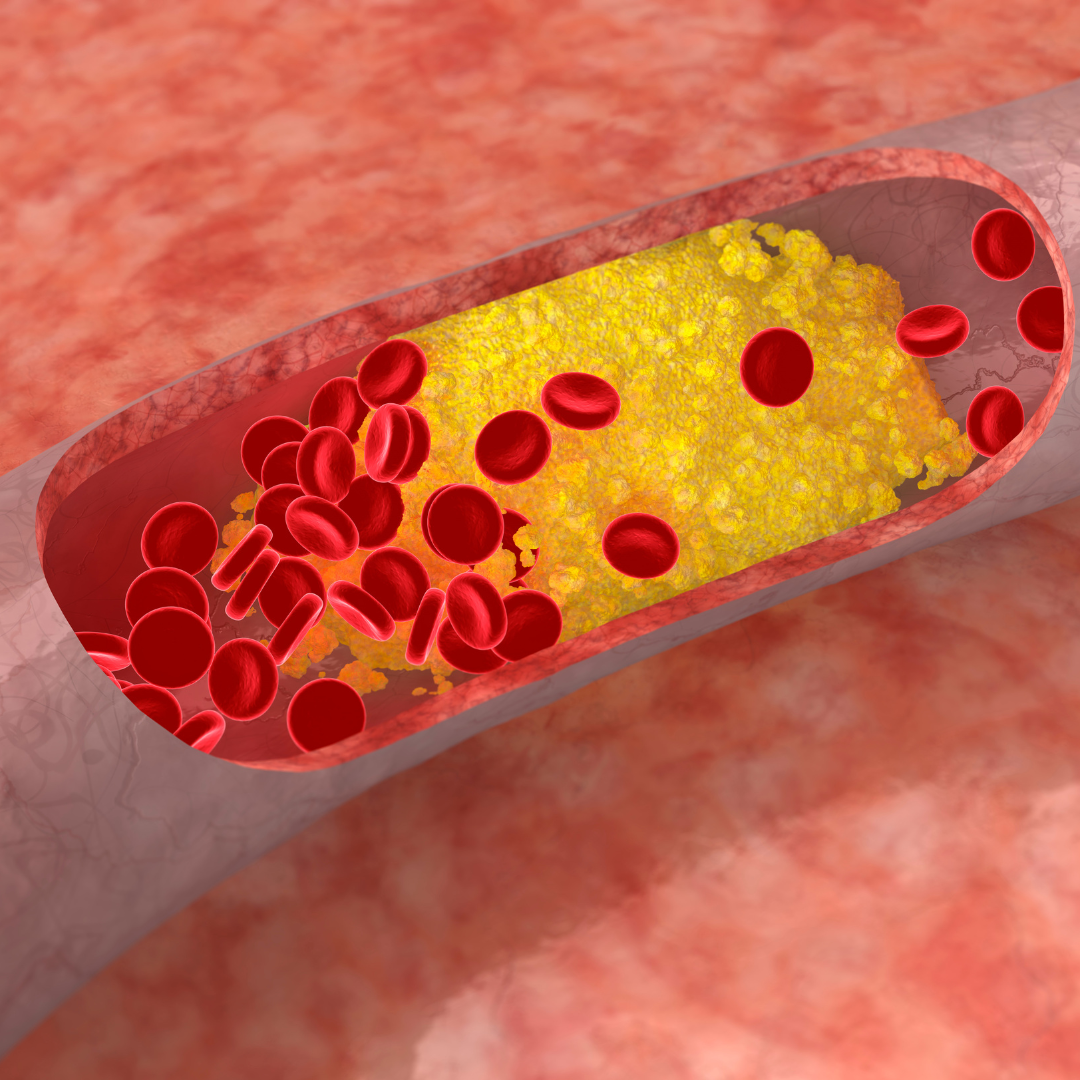
Low-density lipoproteins (LDL) are often referred to as ‘bad’ cholesterol. LDL cholesterol promotes atherosclerosis - the build-up of fatty deposits in blood vessels. This can block blood flow to various parts of the body. In the heart, this could cause a heart attack; in the brain, this could cause a stroke. A diet high in saturated fat is linked to high levels of LDL cholesterol.
The body also contains high-density lipoproteins (HDL) and these are often known as ‘good’ cholesterol. HDL cholesterol helps to remove LDL cholesterol from the body, subsequently reducing the risk of cardiovascular disease. A diet containing unsaturated fats is recommended to promote beneficial levels of HDL cholesterol.

How is menopause linked to metabolic syndrome?
As oestrogen levels reduce with the onset of menopause, fat tends to be stored centrally, around your stomach. Central weight gain is linked to adverse changes in blood lipid levels and blood pressure. It’s this central weight gain that puts women in peri menopause and menopause at greater risk of developing metabolic syndrome.
Falling oestrogen levels are associated with many of the individual issues seen in metabolic syndrome, though it’s still not fully clear whether the primary driver for metabolic syndrome is menopause, insulin resistance or central weight gain. It’s probably enough to know that more women of menopausal age die of coronary heart disease (CHD) than anything else, and that approximately half of those women are affected by metabolic syndrome.
How can you reduce your risk of metabolic syndrome?
While there are some risk factors, such as age and family history that you can’t change, there are many lifestyle habits you can adapt to help reduce your risk of developing metabolic syndrome.
Managing your weight can help prevent excess fat being stored around your middle. Our Back to Basics Menopause Lifestyle and Weight Management programme is equipped to provide you with simple, sustainable lifestyle habits to help not only manage your weight, but support your heart health too. This includes adopting a healthy, balanced diet containing heart friendly unsaturated fats, fibre and plenty of antioxidant rich fruits and vegetables, as well as regular exercise. Reducing your alcohol consumption can also be beneficial, as can stopping smoking.
Hormone Replacement Therapy
There are some differences between different types of Hormone Replacement Therapy (HRT) and the effect they may have on aspects of the metabolic syndrome. All forms of HRT offer some protection or improvement in aspects of the metabolic syndrome. If you are concerned about your risk factors for metabolic syndrome it’s worth discussing this with your HRT prescriber. As with all issues relating to HRT, your prescription needs to be tailored to you, including any individualised risks to, or as a result of, metabolic syndrome.
In summary
Ultimately, developing metabolic syndrome can hinder your quality of life - but it isn’t inevitable . It’s never too early to start making positive changes to reduce your individual risk factors. Nor is it too late to make changes if you are already experiencing the effects of metabolic syndrome. Even small changes can make a big difference.
References
1. https://www.nhs.uk/conditions/metabolic-syndrome/
2. https://www.heartuk.org.uk/genetic-conditions/metabolic-syndrome
3. https://www.rhitrition.com/the-science-of-nutrition
4. https://www.heartuk.org.uk/cholesterol/diabetes
5. https://www.heartuk.org.uk/cholesterol/triglycerides
www.harleystathome.com | Instagram @harleystreetathomemenopause
Facebook: Search Harley Street at Home: Diagnosis, Symptoms & Treatments or Harley St at Home: Lifestyle, Self-Care and Lifestyle to join our private community